Macular Hole
What is a macular hole?
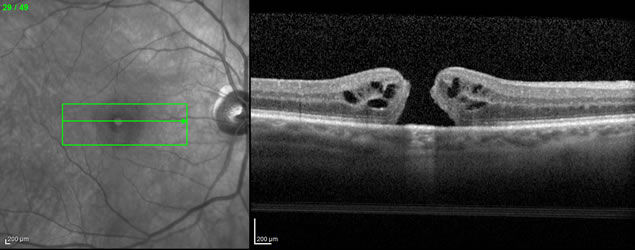 As its name suggests, a macular hole is a hole in the very center of the retina (the macula). Macular holes most commonly affect elderly women, but men can also be affected. About 1 in 10 people who develop a macular hole in one eye will eventually develop a macular hole in the other eye. A macular hole causes gradually progressive blurring and distortion of the central vision. If left untreated, the vision typically worsens to the point of legal blindness (“20/200”) or slightly worse. To the right are images from optical coherence tomography (OCT) showing a macular hole, in “black and white”, as viewed by the examining doctor (left), and in cross-section (right):
As its name suggests, a macular hole is a hole in the very center of the retina (the macula). Macular holes most commonly affect elderly women, but men can also be affected. About 1 in 10 people who develop a macular hole in one eye will eventually develop a macular hole in the other eye. A macular hole causes gradually progressive blurring and distortion of the central vision. If left untreated, the vision typically worsens to the point of legal blindness (“20/200”) or slightly worse. To the right are images from optical coherence tomography (OCT) showing a macular hole, in “black and white”, as viewed by the examining doctor (left), and in cross-section (right):
 The color photograph to the left shows a macular hole, viewed from the perspective of the doctor examining the patient. It is fairly subtle but can be seen in the very center of the image:
The color photograph to the left shows a macular hole, viewed from the perspective of the doctor examining the patient. It is fairly subtle but can be seen in the very center of the image:
What causes a macular hole?
We believe that macular holes are most often caused by pulling forces on the central retina (the macula), caused by the vitreous (the clear gel that fills the back portion of the eye). The hole develops due to separation of tissues rather than a loss of tissue. If you think of the retina like a sheet of cookie dough, it is as though the dough has just been pulled apart to create a hole, as opposed to the dough being removed by a cookie cutter.
How is a macular hole treated?
Until about 1990, there was no known treatment for a macular hole. Today, however, macular holes can be repaired with about a 90% success rate, with visual improvement in most cases. A macular hole is repaired with vitrectomy surgery. Literally, “vitrectomy” means “removal of the vitreous.” If it is still in contact with the retina, the vitreous is peeled from the retinal surface, thus removing the “back-to-front” pulling force. A very thin membrane is often peeled from the retinal surface around the macular hole. Next, the eye is filled with gas that covers the hole for a prolonged period of time to allow the hole to close.
 Since the gas bubble floats to the highest point in the eye, the patient needs to be looking down in order for the gas bubble to be most effectively covering the hole. Most retina specialists recommend face-down positioning for about three to seven days after surgery (not 100% of the time, but close to it!). There is some debate about how crucial face-down positioning is, but it is still recommended by most retina specialists. The image to the right shows how face-down positioning with an intraocular gas bubble facilitates closure of a macular hole:
Since the gas bubble floats to the highest point in the eye, the patient needs to be looking down in order for the gas bubble to be most effectively covering the hole. Most retina specialists recommend face-down positioning for about three to seven days after surgery (not 100% of the time, but close to it!). There is some debate about how crucial face-down positioning is, but it is still recommended by most retina specialists. The image to the right shows how face-down positioning with an intraocular gas bubble facilitates closure of a macular hole:
Refinement of surgical techniques has enabled us to reduce the duration of face-down positioning over the years from about three weeks to one week or less. Fortunately, the overall success rate of closing macular holes has steadily improved since the procedure was introduced in the early 1990’s. Macular holes can be closed without face-down positioning. However, the success rate of this technique may not be quite as high as high as with face-down positioning.
Jetrea (ocriplasmin) is a medication that can be injected into the vitreous for closure of macular holes. Since it can be injected in the office, it enables the patient to avoid the risk and expense of vitrectomy. Jetrea works by releasing the vitreous gel from the macula, so it is intended for cases in which the vitreous is exerting traction on the macula. Jetrea closes macular holes at a much lower rate than vitrectomy. Smaller macular holes with vitreous traction are the best candidates for Jetrea, whereas larger holes and holes without vitreous traction are better candidates for vitrectomy.


