Diabetic Retinopathy
What is diabetic retinopathy?
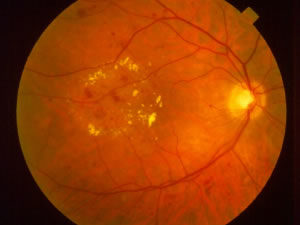
Diabetic retinopathy, as the name implies, is an abnormality of the retina due to diabetes. As a result of damage to the smallest blood vessels in the retina, a variety of problems can arise. There are two types of diabetic retinopathy: nonproliferative and proliferative. Nonproliferative retinopathy (NPDR) is the milder of the two and is identified mainly by small “dots” of blood in the retina. It needs to be monitored closely but often does not cause any visual symptoms. To the right is a photograph showing the macula of a patient with nonproliferative diabetic retinopathy. Notice the scattered red dots; these are small hemorrhages (blood) in the retina. This patient also has macular edema; the yellow spots are known as exudates and are a clue that the retina may be swollen:
The following video provides additional information on nonproliferative diabetic retinopathy (NPDR):
x
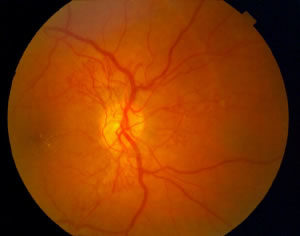 Nonproliferative retinopathy can progress to proliferative retinopathy (PDR), when abnormal blood vessels grow on the surface of the retina. To the left is an example of a patient with proliferative diabetic retinopathy. Notice the fine, lacy blood vessels overlying and extending outward from the optic nerve (the yellowish circle in the center of the photograph):
Nonproliferative retinopathy can progress to proliferative retinopathy (PDR), when abnormal blood vessels grow on the surface of the retina. To the left is an example of a patient with proliferative diabetic retinopathy. Notice the fine, lacy blood vessels overlying and extending outward from the optic nerve (the yellowish circle in the center of the photograph):
The following video provides additional information about proliferative diabetic retinopathy (PDR):
How does diabetic retinopathy cause visual loss, and how is it diagnosed and treated?
Diabetic retinopathy can cause visual loss in several ways. Below is a summary of how diabetic retinopathy can affect the vision, how it is diagnosed and how it can be treated.
1) Macular edema
Macular edema is swelling (“edema”) of the central retina (“macula”). Diabetes damages the small blood vessels within the retina, causing them to leak fluid into the retina. Like a sponge absorbing water, the retina swells. The retina does not function well when it is swollen, so the vision becomes blurred. Macular ischemia, described in detail below, can also cause decreased vision. The following video describes diabetic macular edema and macular ischemia:
When retina specialists detect macular edema on examination, they often obtain a fluorescein angiogram, to identify the areas of leakage and to determine whether there is any lack of blood supply to the macula. The following video describes fluorescein angiography for NPDR:
Optical coherence tomography (OCT) to see the retina in cross-section (as though it is being viewed from the side, rather than from the front) and precisely measure the swelling. The following video provides additional information on OCT for diabetic macular edema:
Macular edema is often treated with laser, in an effort to reduce the amount of swelling. The following video provides additional information about laser treatment for diabetic macular edema.
The main goal of laser treatment for macular edema is to prevent the vision from worsening, although the vision does improve slightly with laser in some cases. When the edema involves the very central part of the retina, injections of medications like Avastin, Lucentis, Eylea, Vabysmo, and steroid injections (Ozurdex, Iluvien, triamcinolone) can reduce the swelling and improve the vision. Avastin and Lucentis are examples of “anti-VEGF” therapy. Triamcinolone, iluvien and Ozurdex are steroids. The following video describes anti-VEGF therapy for PDR:
Sometimes, injections are combined with laser treatment. The photograph of nonproliferative retinopathy above is a good is a good example of macular edema.
2) Vitreous hemorrhage
Vitreous hemorrhage is a result of proliferative diabetic retinopathy. Abnormal blood vessels grow from the retinal surface into the vitreous (a gel that fills the back part of the eye). These vessels sometimes bleed, resulting in a vitreous hemorrhage. The hemorrhage sometimes becomes so dense that it blocks the doctor’s view to the retina. In that case, the doctor will typically use ultrasound to determine whether the retina is attached or detached. The following video provides additional information about ultrasound:
 The photograph on the left shows blood on the surface of the retina known as preretinal hemorrhage, which sometimes precedes a vitreous hemorrhage:
The photograph on the left shows blood on the surface of the retina known as preretinal hemorrhage, which sometimes precedes a vitreous hemorrhage:
Usually, your doctor will allow some time (about a month) for the blood to clear on its own. If it does clear spontaneously, laser treatment called “panretinal photocoagulation” can be done, placing hundreds of small burns in the peripheral retina. The goal of panretinal photocoagulation is to get rid of the abnormal blood vessels. The following video describes panretinal photocoagulation (PRP):
If the blood does not clear significantly after a month or so, your doctor will probably recommend vitrectomy surgery, which would include removal of the blood and vitreous, in addition to panretinal photocoagulation. The following video provides additional information on vitreous hemorrhage:
3) Macular ischemia
Macular ischemia is a lack of blood supply (“ischemia”) to the central retina (“macula”). It is due to closure of the small blood vessels that supply the central retina. Macular ischemia can be identified on a fluorescein angiogram. Unfortunately, there is no specific treatment for macular ischemia.
4) Traction retinal detachment
Traction retinal detachment can result from proliferative diabetic retinopathy. As described above, proliferative retinopathy is defined by abnormal blood vessels that grow from the retinal surface into the vitreous. These vessels cause the vitreous to “stick” to the retina. Sometimes, the vitreous pulls on the retina, creating a “tent” of detached retina. The retina does not function well wherever it is detached. However, unless the detached retina involves the central retina (macula), it does not usually cause visual loss. If the detachment threatens or involves the macula, vitrectomy surgery is performed to re-attach the retina and maintain or restore as much vision as possible. The following video provides additional information on vitrectomy for diabetic retinopathy:


