Choroidal Nevus/Melanoma
What is a choroidal nevus?
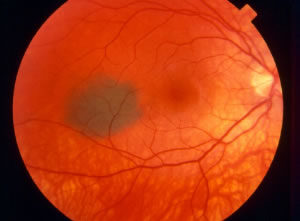
A choroidal nevus is like a mole in the back part of the eye, in a layer called the choroid, which is located behind the retina. It is a benign growth of cells called “melanocytes”. Choroidal nevi (“nevi” is plural for “nevus”) are usually brown and fairly flat, similar to a mole that you might find on your skin. They can be “amelanotic”, lacking the more typical brown color and possessing a more whitish color, instead. The photograph to the right shows a typical choroidal nevus:

What is a choroidal melanoma?
A choroidal melanoma is a malignant (cancerous) growth in the back part of the eye. Like choroidal nevi, choroidal melanomas are usually brown in color, but they can also be amelanotic, with a more whitish color. They can threaten both the vision (by growing and interfering with retinal function) and the patient’s general health (by “metastasizing”, or spreading to other parts of the body). The photograph to the left shows a choroidal melanoma. Notice the large size in contrast to the nevus pictured above. Also, you can probably tell that it is elevated rather than flat:
How can the doctor tell between a nevus and a melanoma?
When a retina specialist identifies an abnormally pigmented lesion in the back part of the eye on a dilated eye exam, he/she looks for various characteristics that help to distinguish between a choroidal nevus and a choroidal melanoma. Nevi can possess some characteristics that are suggestive of a melanoma, so the distinction between a nevus and a melanoma is not always straightforward. A few of these are listed below:
1) Diameter
In general, the smaller the diameter of the lesion, the more likely it is to be a nevus. The larger the lesion, the more likely it is to be a melanoma. Diameter can vary, however, and some melanomas can have a relatively small diameter while nevi can have a relatively large diameter.
2) Height
The flatter the lesion, the more likely it is to be a nevus. The more elevated the lesion, the more likely it is to be a melanoma. Height can vary, also, and some nevi are fairly elevated.
3) Growth
If a lesion grows in diameter and/or height, melanoma will be suspected. However, we do know that some nevi do grow slightly.
4) Subretinal fluid
The presence of fluid over the lesion increases the likelihood that it is a melanoma. However, nevi can be associated with subretinal fluid.
5) Drusen
These are yellowish spots that are sometimes found on the surface of a pigmented choroidal lesion. They are generally a sign that the lesion is benign and more likely a nevus.
6) Orange pigment
The presence of orange pigment on the surface of the lesion is more consistent with a melanoma.
7) Proximity to the optic nerve
This is a risk factor for choroidal melanoma.
8) Visual symptoms
Choroidal melanomas are more likely to cause a problem with the vision. However, nevi can occasionally cause symptoms, as well, particularly if there is overlying subretinal fluid.
Can diagnostic tests distinguish between a nevus and a melanoma?
Yes. Ultrasonography can be used to evaluate a choroidal lesion for characteristics of a melanoma. This test is similar to the ultrasound that obstetricians use to check on a baby in the womb. Some nevi are atypical, meaning that they are not clearly melanoma but possess some characteristics of melanoma. In these cases, ultrasonography can be used to precisely measure the dimensions of the lesion so that it can be closely followed for growth. In addition, ultrasound can be used to assess the internal characteristics of a tumor. Melanoma is characterized by “low internal reflectivity”, meaning that the ultrasound signal from contents of the tumor is low.
What treatments are available for choroidal nevi and melanomas?
Fortunately, only observation, with periodic dilated eye examinations and photographic documentation, is required for choroidal nevi. No treatment is necessary for these benign lesions.
When a choroidal melanoma has been diagnosed, brachytherapy is often recommended. This is a local radiation treatment where a radioactive plaque is placed on the wall of the eye, directly beneath the melanoma, for a few days, and then removed. The placement and removal of the plaque are surgical procedures, performed in an operating room. The plaque delivers radiation in a very focused manner, directly to the melanoma, sparing the rest of the body any significant radiation exposure. Once a choroidal melanoma is diagnosed, the patient will need to be monitored indefinitely for evidence of metastasis to other parts of the body. If metastasis is identified, an oncologist (cancer doctor) will assume responsibility for treatment of the melanoma wherever it has spread.
Can the prognosis for survival of a patient with choroidal melanoma be determined?
Yes. A sample can be taken from the tumor, typically at the time of placement of the radioactive plaque, using a small needle to remove cells. The biopsy can be analyzed using “gene expression profiling”, which provides helpful and reliable information about the potential for metastasis. Based on gene expression profiling, a melanoma can be placed into one of four classes: 1a, 1b, 2a, and 2b. Class 1 tumors are significantly less likely to metastasize than class 2 tumors. The probability of metastasis is very low for class 1a tumors and is slightly higher for 1b tumors. Metastatic risk is significantly higher for class 2a tumors and higher, still, for class 2b tumors.


